Total Unilateral Maxillectomy via a Combined Approach for Resection of a Biologically High-Grade but Histologically Low-Grade Fibrosarcoma
Signalment: 7.5-year-old, MN Siberian husky
History:
This dog presented with a 1-month history of a left-sided muzzle mass. He did not have any other clinical signs associated with this mass.
Physical exam findings:
43.5 mm x 50.4 mm firm and fixed mass extending along the left muzzle from rostral to the orbit to the rostral aspect of the muzzle
No involvement of the oral cavity
Mandibular lymph node normal size on palpation
Diagnostic and clinical staging tests:
CBC: no abnormalities
Serum biochemistry: mildly increased ALT, ALP, and GGT
Punch biopsy: sarcoma
CT scan: left-sided soft tissue mass extending along the lateral aspect of the muzzle. No evidence of either lymph node or lung metastasis.
Treatment:
Total unilateral maxillectomy via a combined dorsolateral skin and intraoral approach, including en bloc resection of the skin overlying the mass. A biologically high-grade but histologically low-grade fibrosarcoma was suspected based on its presentation and CT appearance, so 3 cm soft tissue and bone margins were used for resection, including a rostral orbitectomy. We had initially planned to reconstruct the soft tissue defect with a facial axial pattern flap; however, after resection, this was not required as we were able to preserve the ventral lip margin.
Outcome:
Hi-lo fibrosarcoma with complete excision (skin margins: 7.2 mm to 12.0 mm; bone margins: 6.4 mm to 20.0 mm)
No complications
Video link: https://www.youtube.com/watch?v=6bFNQldai0Q&t=1042s
Tags: #hiloFSA #FSA #orbitectomy #maxillectomy
Preoperative CT scan showing a soft tissue mass extending along the lateral aspect of the left muzzle. This is a more consistent presentation for a hi-lo fibrosarcoma than any other tumor type, and correlated with the preoperative biopsy results.
Preoperative CT scan showing a soft tissue mass extending along the lateral aspect of the left muzzle. There was a small amount of bone involvement (arrow), but otherwise this was entirely a soft tissue mass. This is a more consistent presentation for a hi-lo fibrosarcoma than any other tumor type, and correlated with the preoperative biopsy results.
While the skin overlying the mass was freely movable, this was resected en bloc with the mass because of the high likelihood that this was a hi-lo fibrosarcoma, which is associated with a high risk of local tumor recurrence. Note that the borders for a planned facial axial pattern flap have been marked with a sterile marker pen; however, we did not end up using this flap for reconstruction of the lip defect.
The soft tissue dissection is then continued deeply to the level of the maxilla and full thickness through the lips with 3 cm soft tissue margins in the subcutaneous space.
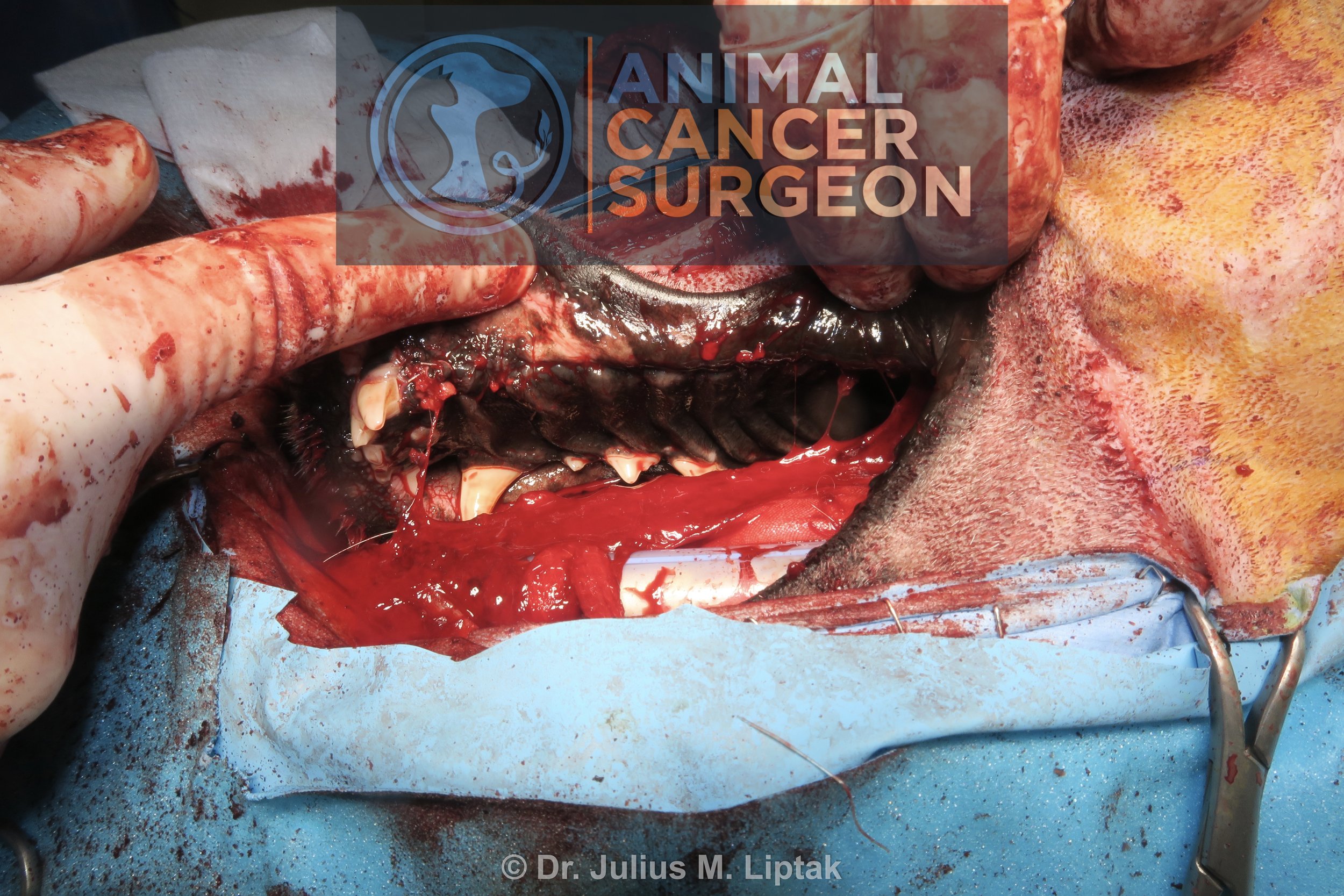
An intraoral incision is made along the gingival margin, connecting the skin incision to create a bipedicle flap (near my left thumb). Pictured is an incision being made along the medial aspect of the dental arcade into the mucoperiosteum of the hard palate.
The mucoperiosteum is then elevated and reflected medially to expose the palatine bone for its osteotomy.
A sagittal saw was used to osteotomize the rostral aspect of the zygomatic arch and caudal maxilla.
A sagittal saw was used to continue the osteotomy along the dorsal midline of the maxilla.
Once the dorsal osteotomy was completed, this was then continued rostrally between the left canine and corner incisor teeth.
The sagittal saw was then used to perform an osteotomy along the hard palate bone.
Finally, an osteotome and mallet were used for the osteotomy within the rostral aspect of the orbit, connecting the dorsal maxilla and palatine osteotomies. This is typically done with an osteotome and done last as this cut has the greatest potential for brisk bleeding from the maxillary artery. While techniques have been described to pre-ligate the maxillary artery, I rarely find this necessary.
Medial soft tissue attachments to the resected maxillary bone are then transected; in this case, with a LigaSure.
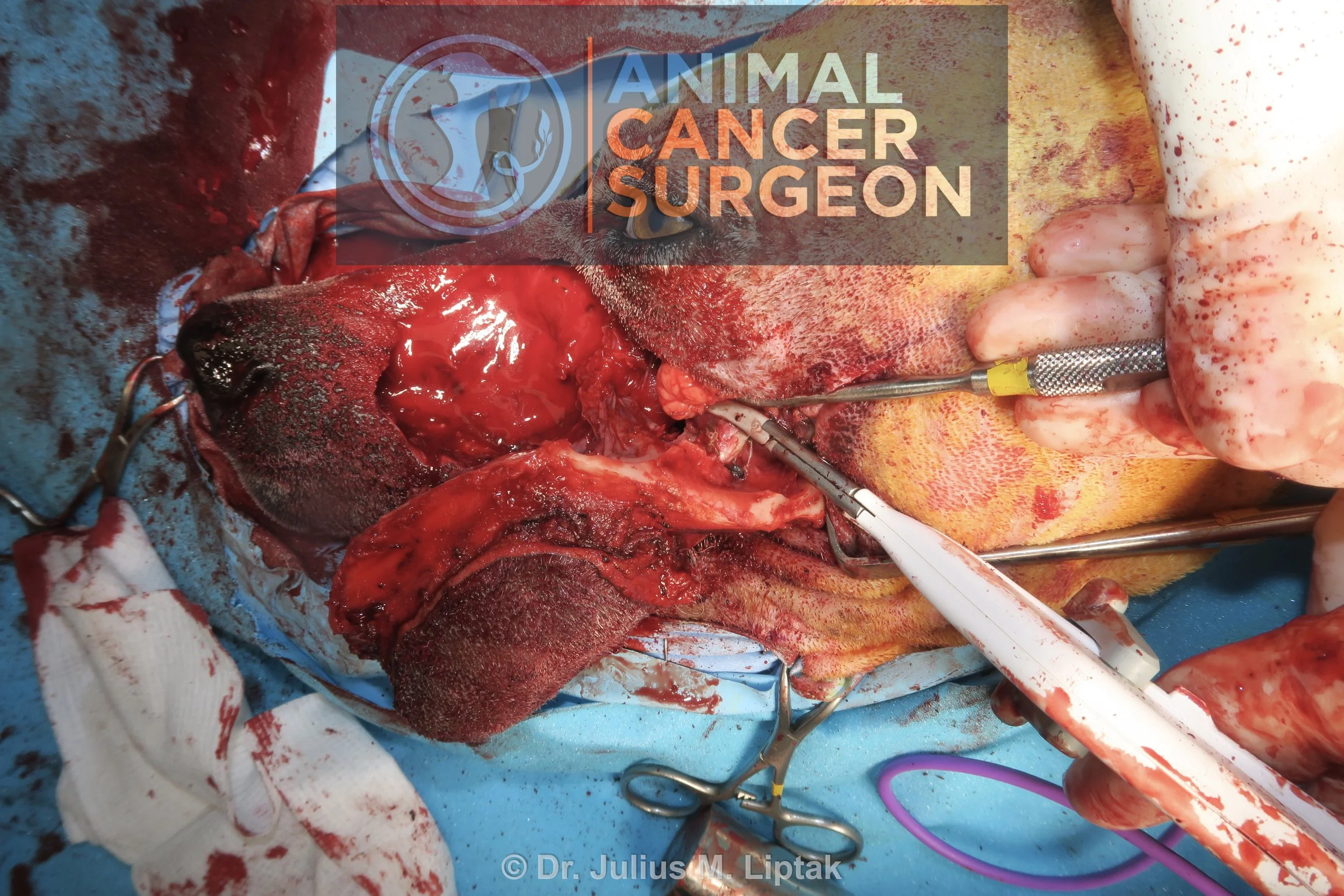
The resected maxillectomy segment immediately prior to being removed from the surgical field.
Appearance of the maxillary defect following removal of the maxillectomy segment for the surgical field.
The mucosa and submucosa of the lip was split to create a labial mucosal-submucosal flap, and then this was sutured to the submucosa of the mucoperiosteum. This is easier to do from the lateral skin incision.
The mucosa and submucosa of the lip was split to create a labial mucosal-submucosal flap, and then this was sutured to the submucosa of the mucoperiosteum. This is easier to do from the lateral skin incision.
Intraoral appearance of the palatine closure.
I had originally planned to close the lateral muzzle defect with a facial axial pattern flap; however, we were able to preserve the ventral aspect of the upper lip and close this defect primarily.
Primary closure of this defect resulted in elevation of the caudal aspect of the upper lip but I preferred this to the potential complications associated with flap reconstruction of this defect.
Postoperative specimen image of the maxillectomy, lateral aspect. This was confirmed as a hi-lo fibrosarcoma with the narrowest histologic tumor-free margins being 6.4 mm.
Postoperative specimen image of the maxillectomy, medial aspect. This was confirmed as a hi-lo fibrosarcoma with the narrowest histologic tumor-free margins being 6.4 mm.
Appearance of the dog 1 day postoperatively.