Reverse Saphenous Conduit Flap for Resconstruction following Wide Resection of a Soft Tissue Sarcoma
Signalment: 11.5-year-old, MN German shepherd
History:
This dog was another tertiary referral after consulting with two surgeons and medical oncologists at two specialty hospitals in Toronto. He first presented to his family veterinarian 3 months beforehand with a12-month history of a slowly growing mass, now measuring 5 cm, ulcerated mass on the dorsal aspect of his left metatarsal region. A thorough workup was done (see below for results), but the dog had also developed a left pelvic limb lameness.
Physical exam findings:
45.8 mm x 48.2 mm ulcerated cutaneous mass on the dorsal aspect of the left metatarsal region; relatively mobile with no palpable invasion into deeper tissues of the metatarsal region
Non-weight bearing left pelvic limb lameness with reluctance and pain on extension of the left hip
Diagnostic and clinical staging tests:
CBC: no significant abnormalities
Serum biochemistry: no significant abnormalities
Three-view thoracic radiographs: no evidence of metastasis
Biopsy: soft tissue sarcoma, grade I
CT scan: L7-S1 intervertebral disc disease with formational impingement on the left side
Notes:
The dog presented to me with a non-weight bearing lameness on the same limb as his soft tissue sarcoma (STS). This is always a concern for me as it raises the possibility that the STS is invasive into deeper structures and causing the lameness. In such cases, the better option is often partial or full limb amputation. In this dog, however, the lameness was more consistent with lumbrosacral disease rather than an invasive STS. As such, a limb amputation would definitely not be the best option for the dog, in fact it would be the worst option for the dog. So a CT was done which confirmed the diagnosis of lumbrosacral disease due to asymmetric, chronic intervertebral disc disease at L7-S1. While waiting for the CT scan, he was started on Metacam and his lameness resolved, which was obviously a good sign as well.
We discussed the different options for management of his STS. Wide resection was recommended as marginal resection would still result in the need to reconstruct the wound; if the wound needs to reconstructed regardless, then it is best to do a wide resection to increase the chance of a complete histologic excision and decrease the risks of contaminating the defect and any reconstructive effort to reconstruct the defect. These options included second intention healing, singe-session resection and reconstruction with a reverse saphenous conduit flap, staged resection and reconstruction with a free-meshed skin graft, and staged reconstruction with a direct distant hinge flap. The latter was ruled out because of his lumbrosacral disease (although I do prefer this to free-meshed skin grafts), and the single-session reconstruction was preferred because the owners were from 5 hours away.
Treatment:
Wide resection of the STS, including digit extensor tendons for deep margins (yes, this is well tolerated!), and reconstruction of the defect with a reverse saphenous conduit flap. In addition, he received an epidural injection of methylprednisolone acetate to treat his lumbrosacral disease.
Outcome:
Soft tissue sarcoma, grade II; complete histologic excision with 7.9 mm and 4.9 mm histologic tumor-free lateral and deep margins
Distal flap incisional dehiscence followed 2 days later by complete flap necrosis and failure, possibly secondary to a bandage placed to manage the incisional dehiscence
Acute and rapid lumbrosacral disease deterioration with non-ambulatory paraparesis and urinary incontinence
Euthanasia 12 days postoperatively :(
Notes:
The grade shift between preoperative biopsy and definitive histopathology is not uncommon. In one study, 39% of dogs had a different histologic grade on their definitive histopathology compared to their preoperative biopsy, usually a grade higher than the biopsy.
I suspect that this dog’s flap necrosis started as a result of the bandage strangulating the median saphenous vein and caudal saphenous artery at the tibiotarsal joint. Prior to this, the flap showed no signs of vascular compromise with no bruising or necrosis. The bandage was necessary and it was just an unfortunate series of events.
I have not seen a dog with lumbrosacral disease deteriorate so rapidly before, and this was the ultimate reason for the owners electing euthanasia. We could have debrided the necrotic flap and managed the wound with second intention healing or a free-meshed skin graft; however, his lumbrosacral disease would have required a dorsal laminectomy with distraction-fusion, and this, combined with managing his wound, was a lot to put an old dog through.
Video link: https://www.youtube.com/watch?v=LYq6AscmM10
Tags: #STS #softtissuesarcoma #reconstruction #reversesaphenousconduitflap #complications #IVDD #LSdisease
The STS on the dorsal aspect of the left metatarsals with the borders of the reverse saphenous conduit flap marked with a sterile marker pen. The base of the flap is the medial malleolus, the caudal border is along the caudal aspect of and parallel to the tibia, the cranial border is along the cranial aspect of and parallel to the tibia, and the proximal border, in this dog, connected the cranial and caudal borders immediately distal to the level of the patella.
The flap was raised before resection of the STS with incisions along the proximal, cranial, and caudal borders of the flap. The saphenous artery and vein were sealed and transected with a LigaSure near to the proximal aspect of the flap, and the flap was undermined deep to the subcutaneous tissue.
During dissection, a segment of the medial gastrocnemius fascia was raised with the flap to protect the median saphenous vein and caudal saphenous artery.
The reverse saphenous conduit flap was raised in a proximal to distal direction, preserving the tibial nerve caudally.
The flap donor site was then closed prior to wide resection of the STS to minimize the risk of contaminating the flap donor site with tumor cells.
Appearance of the raised reverse saphenous conduit flap following closure of the donor site.
A bridging incision was then done to connect the flap donor site and the planned defect following resection of the STS.
The STS was resected with 1.5 cm lateral margins.
Deep margins were extended to the metatarsal bones, including the digit extensor tendons and joint capsule of some of the metatarsophalangeal joints.
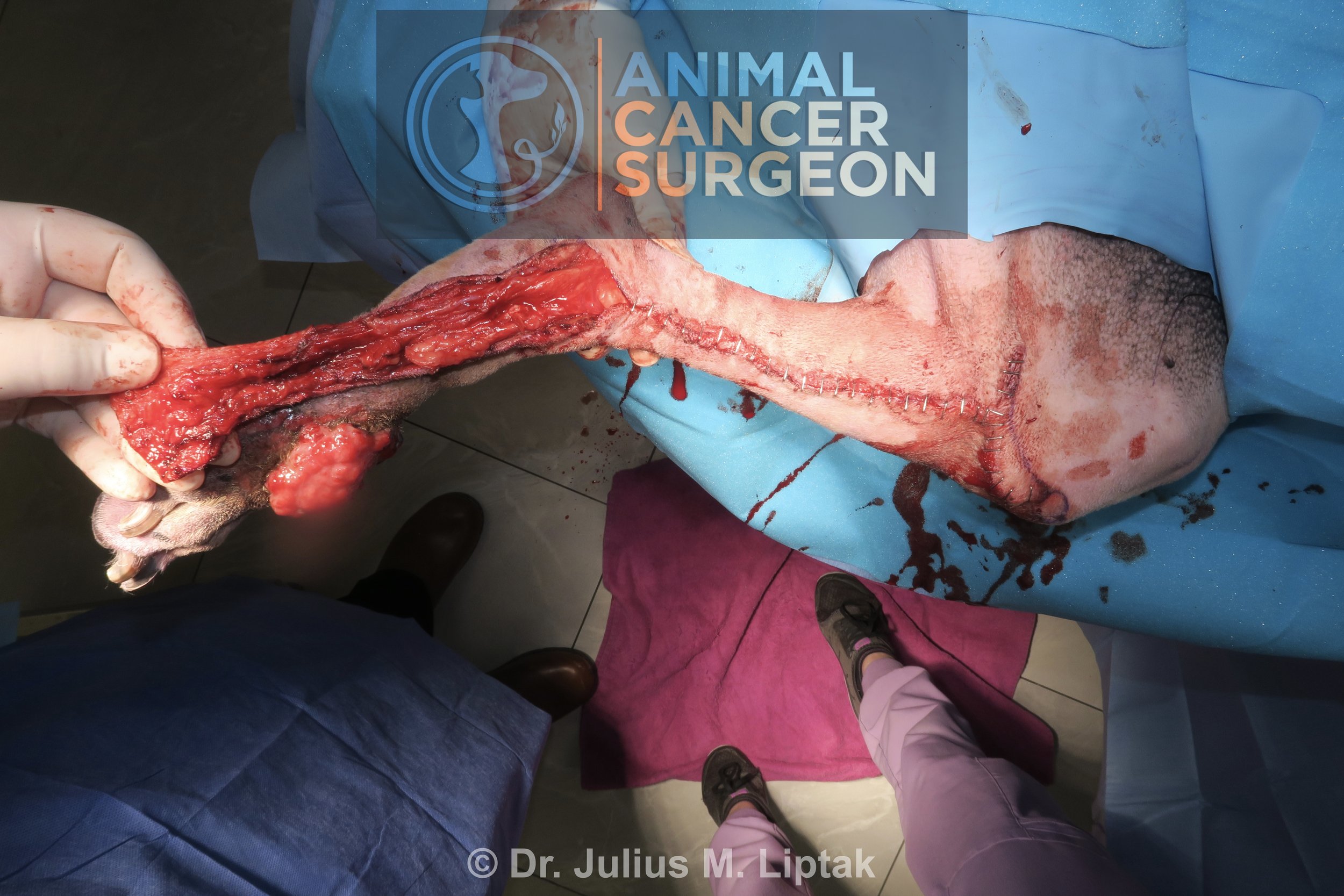
The reverse saphenous conduit flap was then transposed into the defect.
After transposition, the reverse saphenous conduit flap was secured into the defect in two layers, a 3-0 Monocryl simple continuous suture pattern in the subcutaneous layer and staples in the skin.
Appearance on postoperative day 1. There is mild bruising but the flap was warm throughout. Note the position of the proximal flap with the hock flexed. I think this, in combination with the bandage, may have played a role in strangulating the median saphenous vein and caudal saphenous artery at the tibiotarsal joint later in the postoperative period.
Two days postoperatively, the distal aspect of the flap had incisional dehiscence. There is some deeper bruising along the distal aspect of the flap.
Four days postoperatively, there is some necrosis of the distal aspect of the flap (arrows) but the remainder of the flap appears relatively healthy with no evidence of impending doom, which I would usually expect to see by this stage with typical distal flap necrosis.
This is the more concerning image because there is tissue necrosis at the junction of the distal aspect of the flap donor site and the proximal aspect of the bridging incision.
The distal aspect of the flap was debrided and closed primarily. This was closed with as little tension as possible because tension at the distal aspect of the flap can reduce partial pressures of oxygen and lead to further flap necrosis.
The appearance of the flap three days later, seven days postoperatively. Very, very sad. This is not a typical progression or timing for flap necrosis, so I suspect the bandage may have exacerbated pressure at the hock joint when in flexion and resulted in compression of the the median saphenous vein and caudal saphenous artery at the level of the tibiotarsal joint.
Appearance of the flap 10 days after surgery.