lung carcinomas
BACKGROUND
Lung tumors are uncommon in both cats and dogs. The most common primary lung tumor is a bronchoalveolar carcinoma, although histiocytic sarcomas are also considered primary lung tumors. Primary lung tumors can either be an asymptomatic incidental findings (30%) or associated with clinical signs (70%) such as coughing, lethargy, and respiratory difficulties in dogs. Occasionally dogs with a primary lung carcinoma will present with a paraneoplastic syndrome such as hypertrophic osteopathy or hypercalcemia.
Cats are often symptomatic and present with similar clinical signs as dogs. However, cats also can present with lameness because of so-called lung-digit syndrome (or acrometastasis) as well as monoparesis as a result of arterial embolization. In one study of 36 cats with digit metastasis from primary lung carcinomas (2000), common clinical signs included swelling and/or ulceration of the digit, or deviation or loss of the nail. Multiple digit involvement was reported in 17% of cats. The weight bearing digits were involved in 75% of cats, and radiographically all cats had lysis of the third phalanx of the affected digit.
DIAGNOSIS
Thoracic radiographs or CT scans are required for diagnosis and clinical staging. Primary lung tumors are typically well-circumscribed solitary masses in dogs, but are more difficult to diagnose in cats. In cats, three radiographic patterns consistent with primary lung carcinomas have been described: mixed bronchoalveolar pattern, ill-defined alveolar mass, or mass with cavitation. Pleural effusion is also a relatively common finding in cats with primary lung carcinoma (33% of cats in one study). Primary lung carcinomas have a predilection for the caudal lung lobes, while histiocytic sarcomas most commonly involve the left cranial or right middle lung lobes, have internal air bronchograms on radiographs (whereas both carcinomas and sarcomas have internal air bronchograms on CT scans), and are larger than primary lung carcinomas. Ultrasound-guided fine-needle aspirates are occasionally recommended for definitive diagnosis, but this is rarely required because the diagnosis (ie, tumor, abscess, etc) does not change the recommended treatment of lung lobectomy. Furthermore, there are risks associated with fine-needle aspiration (such as tumor seeding, pneumothorax, hemothorax, etc) and, in one study, 63% of aspirates were non-diagnostic.
CLINICAL STAGING
Thoracic CT scans are preferred for clinical staging as they are more sensitive for the detection of metastatic disease. In a 2011 imaging study of 19 dogs with primary lung tumors staged with thoracic CT scans, 21% of dogs had suspected lymph node metastasis and 26% had suspected lung metastasis. In another clinical study (2006), based on tracheobronchial lymph node size alone, the ability of thoracic CT to correctly assess the status of the tracheobronchial lymph nodes as metastatic or non-metastatic had an 83% sensitivity (with one false-negative result), 100% specificity, 100% positive predictive value, and 89% negative predictive value. The CT appearance of tracheobronchial lymph nodes correlates with metastastic disease in another clinical study (2010) with lymph node metastasis very likely with maximal lymph node diameter > 12mm, lymph node-to-thoracic body ratio of 1.05, and heterogenous and/or ring contrast enhancement pattern.
TREATMENT
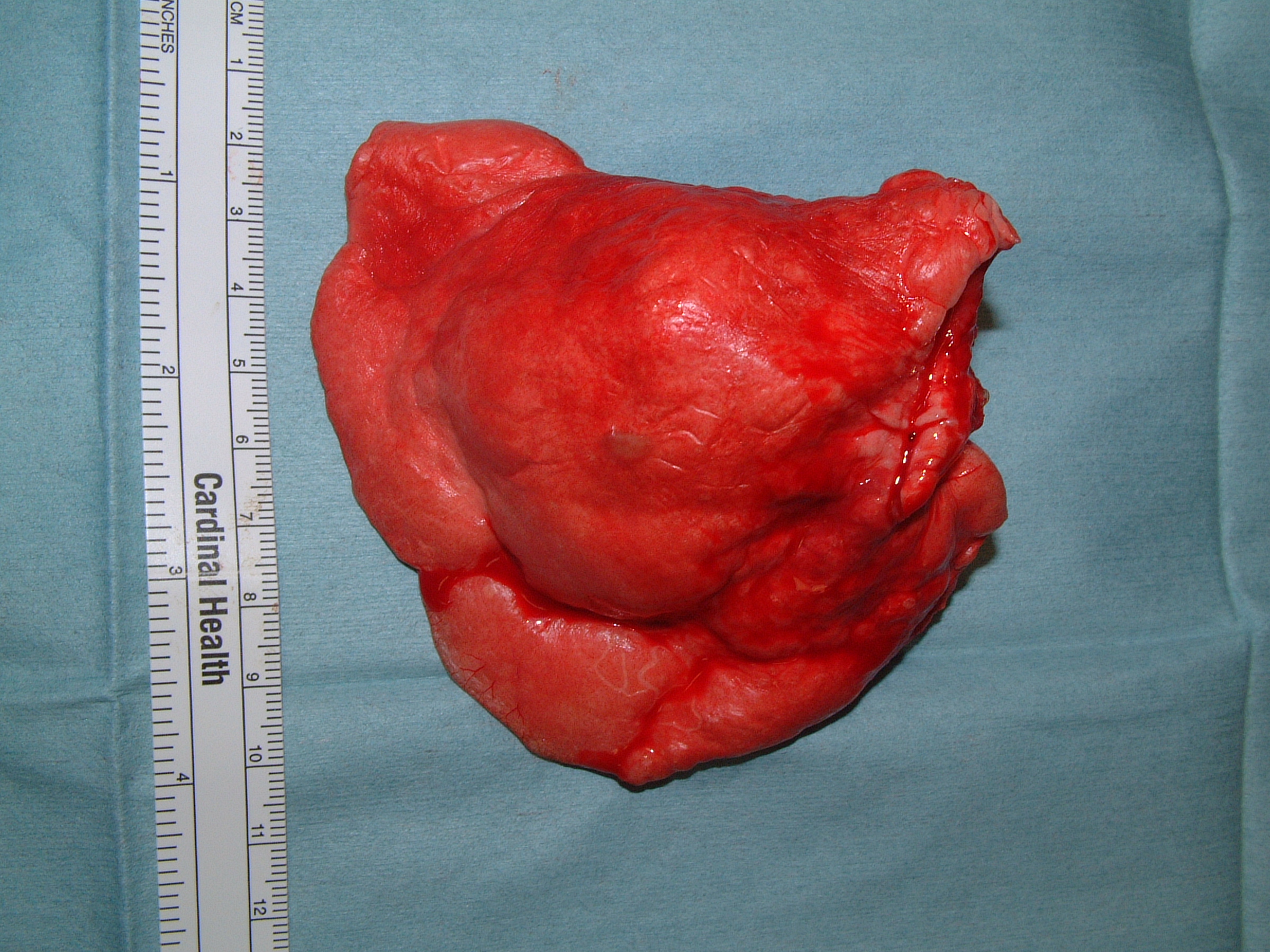
Lung lobectomy is recommended for the removal of lung tumors. Lung lobectomy is usually performed via an open intercostal thoracotomy approach and is associated with a low risk of perioperative complications. Rarely, more extensive procedures are required for resection, such as pneumonectomy. Thoracoscopic lung lobectomy has been described, but this is only performed in a few academic hospitals and, despite being performed for small primary lung tumors (2.0cm-2.7cm), there was a 23% conversion rate to open thoracotomy.
Chemotherapy should be considered for all cats with lung tumors and dogs with grade III carcinomas or lymph node metastasis. Chemotherapy options may include carboplatin, navelbine, and tyrosine kinase inhibitors.
PROGNOSIS
Dogs
In one clinical study of 67 dogs with surgically excised primary lung carcinomas (1997), the overall median survival time was 361 days. Prognostic factors included clinical signs, clinical stage, tumor type, and histologic grade. Dogs with clinical signs associated with their primary lung tumor had a median survival time of 240 days compared to 545 days for asymptomatic dogs. Dogs with single solitary lung tumors (T1 clinical stage) had a median survival time of 790 days, which was significantly longer than dogs with multiple lung tumors (T2 clinical stage, 196 days) and dogs with lung tumors invading into adjacent structures (T3 clinical stage, 81 days). The median survival time for dogs with no evidence of lymph node metastasis (N0) was 452 days and this was significantly longer than the median survival time of 26 days for dogs with tracheobronchial lymph node metastasis (N1). Finally, the median survival time for dogs with grade I lung carcinomas was 790 days and this was significantly longer than the median survival times of 251 days and 5 days for dogs with grade II and III lung carcinomas, respectively. In other studies, tumor size, tumor location within the lung lobe, and tumor type were also prognostic. The mean survival times for dogs with primary lung carcinomas < 5cm was 20 months compared to 8 months for dogs with tumors > 5cm. The mean survival time for lung tumors involving the entire lung lobe was 8 months compared to 12 months for primary lung carcinomas involving the periphery of the lung lobe. The median survival time for dogs with squamous cell carcinoma, which is rare, was 8 months compared to 19 months for dogs with adenocarcinoma.
Cats
The prognosis is guarded to poor for cats with primary lung carcinomas. In one clinical study of 21 cats traeted with lung lobectomy (1998), the overall median survival time was 115 days. The only prognostic factor in this study was histologic grade. The median survival time for cats with moderately differentiated carcinomas was 698 days compared to only 75 days for cats with poorly differentiated carcinomas. Radiographic evidence of tracheobronchial lymph node enlargement may have prognostic significance in cats with a median survival time of 412 days for cats with normal sized lymph nodes, but 73 days in cats with enlarged lymph nodes. The median survival time for 36 cats with digit metastasis was 67 days.
Last updated on 6th March 2017